 Industry
Industry

![]() Health Care
Health Care
 Products
Products


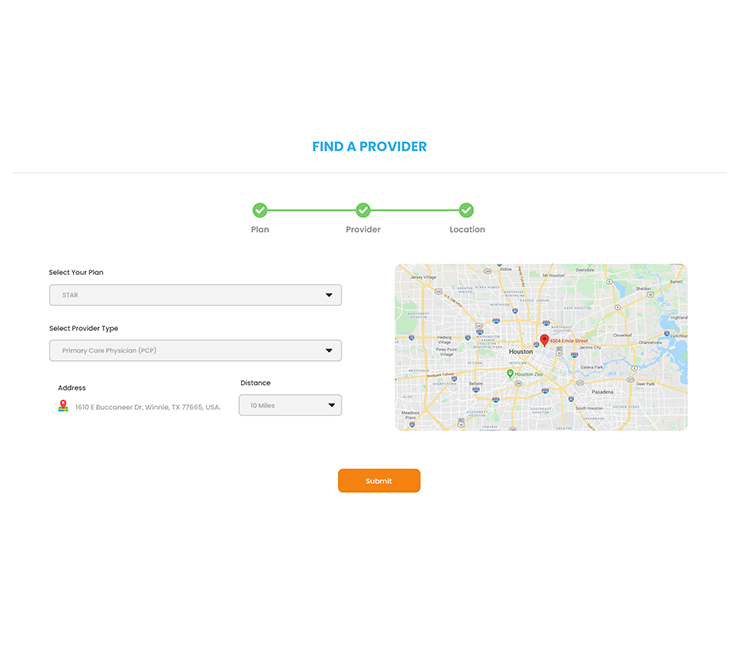
Health Cloud - Find a Doctor
Overview
- The Find A Doctor tool has been developed with the purpose of helping patients locate medical practitioners within their designated area, and it currently stands as the largest referral network in the field.
- In the Health Industry, one of the crucial functionalities is the ability for patients to search and find doctors based on their specific needs and requirements. This feature plays a significant role in facilitating the process of connecting patients with the most suitable healthcare providers.


Problem Statement
- The existing functionality within the Community Portal fails to provide a seamless and efficient process for patients/members to search for nearby practitioners based on their insurance plan and obtain comprehensive details about those practitioners. This limitation creates challenges for patients/members who are seeking convenient access to healthcare services that align with their insurance coverage and require detailed information about potential practitioners.
Solution
Gather the details of the patient, to achieve the requirement of finding a nearby doctor,
- For searching the doctors/ practitioners, the patient has to choose the Insurance plan details, and what type of Provider they are looking for, like whether the Service provider is either.
- Primary Care Physician
- Specialist
- Hospital
- Urgent Care
- Facility
- Also, the patients can select their location details, so that the registered Provider results are displayed based on the nearby location of the patient
- Therefore, based on the evaluation of the details, displayed the results of Practitioners, by sorting the nearby doctors on top and rest available locations.
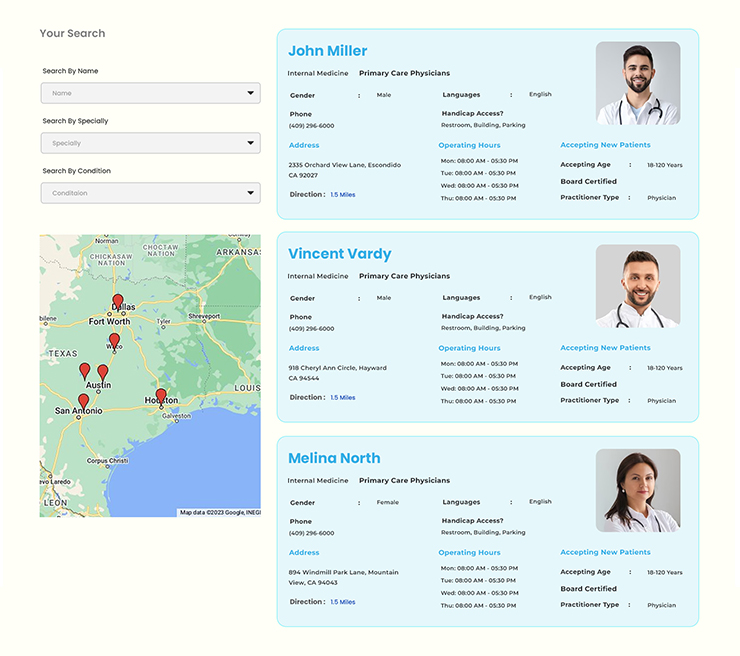
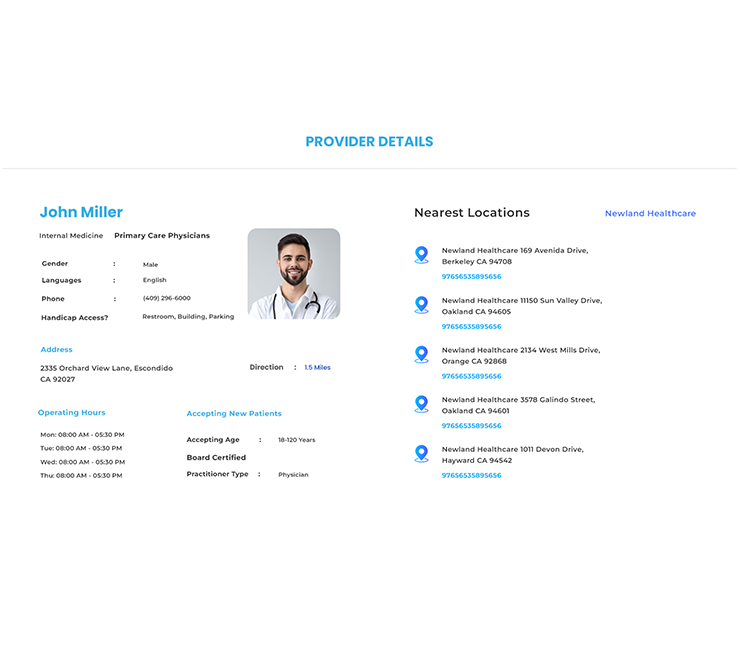
- Results also added with details like
- Address of the provider
- The specialty of the provider
- Languages are known by the Practitioners
- Certifications that the provider has completed.
- Operating hours in that location will also be available,
- Panel Status (whether they accept new patients or not)
- Gender details
- Contact details with available for Telehealth and Telemedicine information
- Parking facilities available in the Provider’s location
- Handicap Access details
- Also, it has other features to get results based on other optimized filters like whether practitioners are available on weekends and based on required Specialities.
Business Benefit
- Implementing an enhanced functionality within the Community Portal to allow patients/members to easily find nearby practitioners based on their insurance plan and access practitioner details can bring several significant benefits to the business:
- Improved Member Satisfaction
- Increased Utilization of Network Providers
- Enhanced Retention and Loyalty
- Reduced Administrative Workload
- Data Insights and Analytics
- insurance plan utilization, and practitioner selection, the business can gain valuable insights. These insights can be used to optimize network provider contracts, tailor marketing efforts, and improve the overall quality of care provided.
Health Cloud - Prior Authorization
Overview
Prior authorization is a management procedure used by insurance providers to decide whether to cover a certain product or service. It involves assessing whether the cost of the product or service will be fully or partially covered. This procedure is commonly applied to various treatments, surgeries, or services prior to their provision to the patient.

Problem Statement
The current process for provider staff to raise requests to insurance companies and gather patient details regarding insurance plans, diagnoses, and procedures lacks efficiency and a centralized system. This poses challenges in effectively accessing and managing the necessary information through the Community Portal.
Provider staff often struggle with the existing process of submitting requests and retrieving patient-related details for insurance purposes. This can result in delays, errors, and inconsistencies, leading to potential disruptions in the healthcare workflow and reimbursement processes.
Solution
To streamline the prior authorization process and improve efficiency for practitioners or provider staff, a comprehensive solution can be implemented.
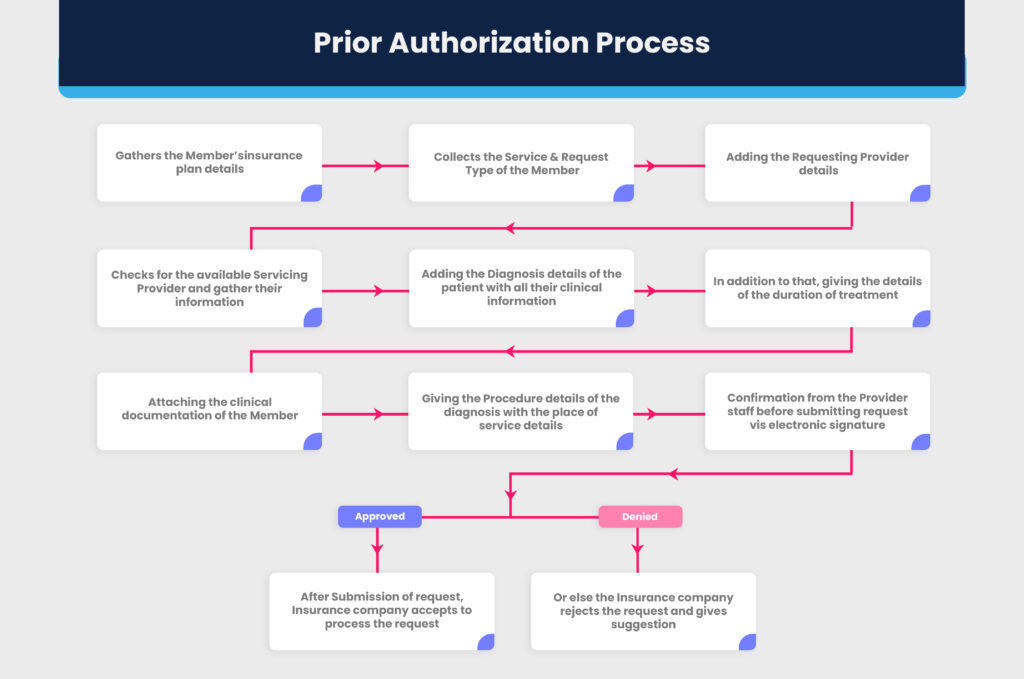
- Prior Authorization is a process by which the practitioners or provider staff of the Hospital raise a request to the insurance companies about the cost and insurance coverage of the diagnosis of the specified treatment to the patient before commencing it. After the approval of the Insurance company, the request will be getting processed by the Provider staff.
- Initially, the provider will gather the details of the Patient’s diagnosis and their Insurance Member plan and its coverage details. Based on the plan details they will check whether the diagnosis treatment is available in their Organization and check for the available Practitioners who practise it.


- The Provider staff raise a Care request based on the Member’s(patient) service authorization and request type. Also gathers the details of the Care Diagnosis, time period to complete the treatment, stay details, clinical information and clinical documents of the member.
- Verifies the Health Care Procedure for the diagnosis and gathers the details of the healthcare place of services. After gathering all the procedure details for the diagnosis of the Member’s plan type, verifies a confirmation from Provider staff who raise the care request.
- This request will be submitted to the insurance provider, where they check and analyse to approve or reject. If the request gets approved, it will be notified to the Hospital organization and treatment process gets commenced or if it gets rejected, the insurance provider suggests another similar procedure or plan or health care organization that covers or relates for the treatment.
Benefit
- Improved Financial Predictability
- Enhanced Treatment Timeliness
- Reduced Denials and Appeals
- Streamlined Administrative Processes
- Enhanced Provider-Insurer Collaboration
- Increased Patient Satisfaction
- Mitigated Financial Risks
These business benefits help create a more efficient and transparent healthcare system.




 .
.